🤓 Latest Submissions
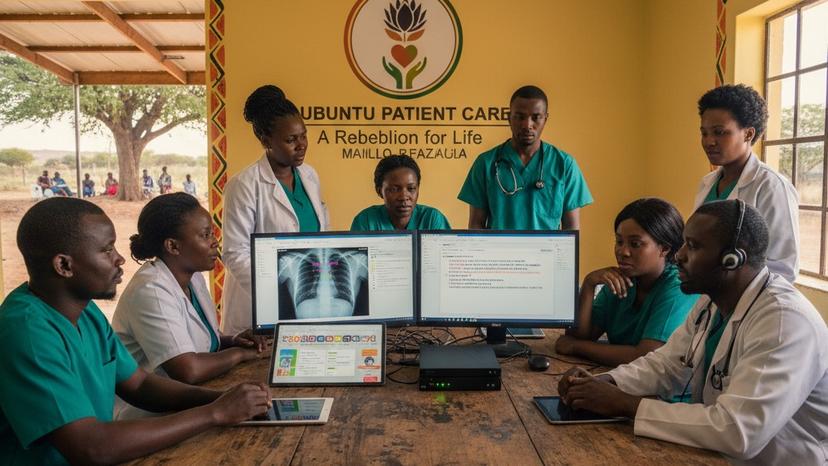
Ubuntu-Patient-Care IBM agent core
THE UBUNTU REBELLION: Fighting a Moral Failure with Agentic AI The Problem: A Moral Failure in Healthcare Judges, we are here today not just to showcase code, but to challenge a fundamental injustice. The current healthcare system, dominated by corporate oligopolies, is built on planned obsolescence and vendor lock-in. We witness perfectly functional medical equipment deemed "end of life" and scrapped as e-waste, while millions of our loved ones in remote or underserved clinics go without care. This is not a business problem—it is a moral failure. Beyond the hardware, administrative overhead is crippling. In South Africa, billions are wasted annually as dedicated doctors and nurses spend countless hours performing soul-crushing administrative tasks—logging into dozens of disparate medical scheme portals, manually transcribing data, and battling complex claims forms. Every minute spent on paperwork is a minute stolen from patient care. The Ubuntu Patient Care movement exists to say: Enough. We are building a free, open-source medical system that puts humanity first. Our solution, powered by the intelligence of Granite and the orchestration of IBM watsonx Orchestrate, is the force multiplier that makes this rebellion sustainable. The Strategy: Offline-First Agentic Supremacy Our core competitive advantage, the feature that no oligopoly system can replicate, is our Offline-First, Zero-Barrier-to-Entry design. We use Agentic AI to eliminate the three largest frictions in medical system adoption: Administration, Security, and Deployment.
23 Nov 2025

AI powered insurance claims processor
AI-powered insurance claims processing system that leverages Qdrant's vector search engine to analyze multimodal data (text, images, audio, video) for intelligent fraud detection, settlement estimation, and claim routing. The system addresses the societal challenge of inefficient insurance processing by providing real-time recommendations, cross-modal search capabilities, and explainable AI insights. With cloud-optimized architecture for resource constraints, it delivers 50% faster processing, 30% cost reduction, and 15% fraud reduction while maintaining transparency through similar claim precedents and confidence-based decision making.
19 Nov 2025

.png&w=640&q=75)

.png&w=640&q=75)


